The Diabetic Eye
Diabetes is a disease that occurs when the pancreas does not secrete enough insulin or the body is unable to process it properly. Insulin is the hormone that regulates the level of sugar (glucose) in the blood. The disease can wreak havoc on the body and its organs, including the eyes. Patients with diabetes are more likely to develop eye problems such as cataracts, glaucoma, diabetic retinopathy and macular edema. Diabetic retinopathy is the main threat to vision.
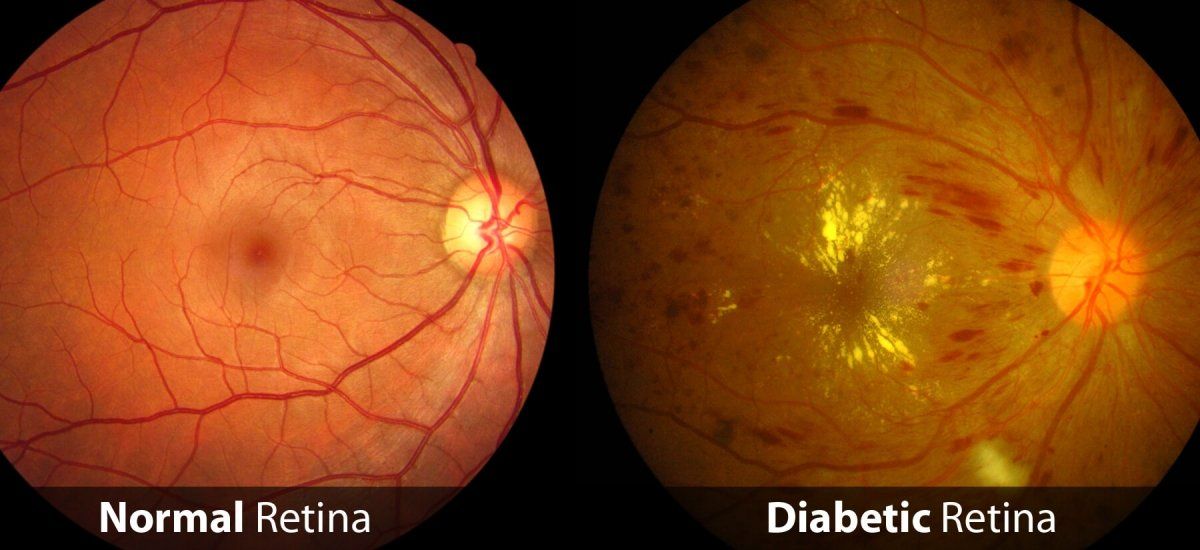
Over time, diabetes affects the circulatory system of the retina. The earliest phase of the disease is known as background diabetic retinopathy. In this phase, the arteries in the retina become weakened and leak, forming small, dot-like hemorrhages. These leaking vessels often lead to swelling or edema in the retina and decreased vision.
The next stage is known as proliferative diabetic retinopathy. In this stage, circulation problems cause areas of the retina to become oxygen-deprived or ischemic. New fragile vessels develop as the circulatory system attempts to maintain adequate oxygen levels within the retina. This is called neovascularization. Unfortunately, these delicate vessels hemorrhage easily. Blood may leak into the retina and vitreous, causing spots or floaters, along with decreased vision.
In the later phases of the disease, continued abnormal vessel growth and scar tissue may cause serious problems such as retinal detachment and glaucoma.
The effect of diabetic retinopathy on vision varies widely, depending on the stage of the disease. Some common symptoms of diabetic retinopathy are listed below, however, diabetes may cause other eye symptoms.
- Blurred vision (this is often linked to blood sugar levels)
- Floaters and flashes
- Sudden loss of vision
The diagnosis of diabetic retinopathy is made following a detailed examination of the retina with an ophthalmoscope. Most patients with diabetic retinopathy are referred to vitreo-retinal surgeons who specialize in treating this disease. Diabetic retinopathy is treated in many ways depending on the stage of the disease and the specific problem that requires attention.
It’s important to manage your diabetes with the help of an internist or an endocrinologist along with a qualified ophthalmologist. Maintaining a healthy lifestyle; including managing blood sugars and keeping A1C in check along with routine monitoring with your eye doctor are the best ways to help preserve your best vision while living with diabetes.
At Talley Eye Institute, we offer the benefit of having multiple specialties under one roof; from consultative optometry to comprehensive ophthalmology, vitreo-retinal and glaucoma treatment to cataract surgery. Our team of board-certified ophthalmologists are highly skilled and experienced in treating diabetic eye diseases. If you are living with diabetes and haven’t yet become established with an eye doctor, give us a call today to schedule an exam.