DIABETIC RETINOPATHY
DIABETIC RETINOPATHY
What is diabetic retinopathy? How does it form?
What is diabetic retinopathy? How does it form?
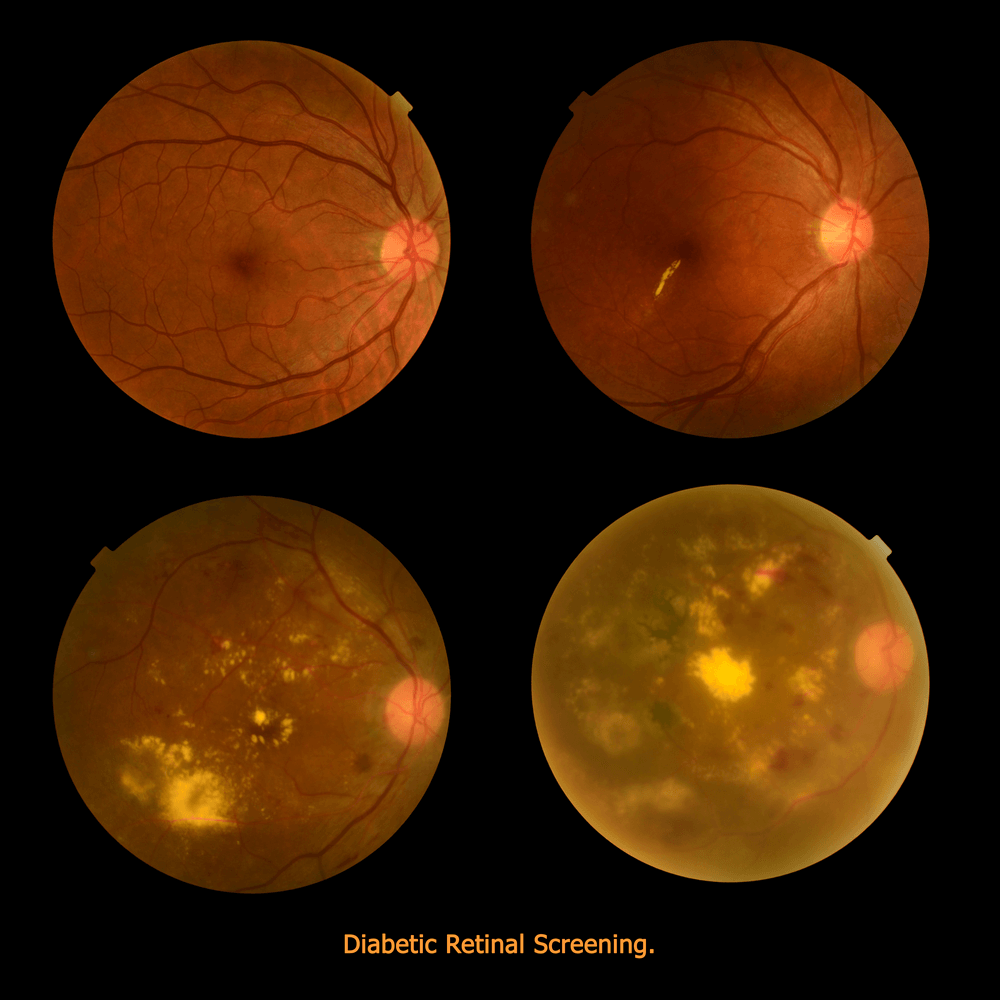
The medical field is still learning how diabetes leads to so many problems within the body. We know that sugar control reduces the risk of problems in the body and that holds true within the eye as well. Diabetes affects a very important structure of the eye that is responsible for vision called the retina. When we see changes to the retina from diabetes this is called diabetic retinopathy.
After many years of elevated blood sugars, the vasculature to the eye becomes less and less effective at delivering nutrition. Vessel walls may weaken and even break. Microscopic spots of blood appear on the surface of the retina and can be seen during a dilated eye exam. The number and location of these spots of blood is used to grade the degree of retinopathy and assess the risk for future vision loss.
How Does Diabetes Affect The Retina?
There are several ways diabetic disease can lead to vision loss. One cause is related to diabetic retinopathy. Over time the blood vessels in your retina become less effective at delivering oxygen and nutrition. This reduction in oxygen and nutrition to the retina causes tissue death. In an effort to survive, the retina stimulates the release of small chemical in the eye called VEGF which promotes new blood vessel formation. These new blood vessels are fragile and poorly built. They eventually break and bleed into the eye. Bleeding into the eye is a common cause of significant vision loss in patients with diabetes.
In addition to bleeding, these new blood vessels can also contract or shrink. If this happens it can pull and lift the retina up causing a “tractional” retinal detachment. This is another cause of vision loss and it can be associated with significant vision loss that requires surgery. Even after repair the visual outcome is often poor with limited visual recovery.
Another reason for vision loss is related retinal atrophy or tissue loss that occurs after years of poor blood flow. Usually the retinal atrophy happens along the outside wall of the eye which is responsible for peripheral vision, however it can also happen in the macula which can be associated with central vision loss.
One of the more common causes of vision loss is related to macular edema, or swelling. This is usually located in the area of your eye that is responsible for your central vision, the macula. The disruption of the tissue from the swelling leads to reduced vision. If left untreated, over months it can lead to tissue remodeling and permanent vision loss.
Signs And Symptoms
The effect of diabetic retinopathy on vision varies widely, depending on the stage of the disease. Some common symptoms of diabetic retinopathy are listed below, however, diabetes may cause other eye symptoms.
- Blurred vision (this is often linked to blood sugar levels)
- Floaters and flashes
- Sudden loss of vision
Detection And Diagnosis
Diabetic patients require routine eye examinations so related eye problems can be detected and treated as early as possible. Most diabetic patients are frequently examined by an internist or endocrinologist who in turn work closely with the ophthalmologist.
The diagnosis of diabetic retinopathy is made following a detailed examination of the retina with an ophthalmoscope. Most patients with diabetic retinopathy are referred to vitreo-retinal surgeons who specialize in treating this disease.
Prevention
Researchers have found that diabetic patients who are able to maintain appropriate blood sugar levels have fewer eye problems than those with poor control. Diet and exercise play important roles in the overall health of those with diabetes.
Diabetics can also greatly reduce the possibilities of eye complications by scheduling routine examinations with an ophthalmologist. Many problems can be treated with much greater success when caught early.
Treatment
During the early stages, diabetic retinopathy can be monitored. Often times good sugar control can delay the progression of diabetic changes in the eye. However, as the disease progresses treatments such as injections of medicine in the eye and/or laser treatment may be recommended.
Surgical options for patients with diabetic retinopathy:
The typical patients requiring surgery usually have advanced disease called proliferative diabetic retinopathy or PDR. In PDR the retina is “starved” for oxygen and the body responds by producing new blood vessels to try and help provide oxygenation and nutrition. But these new blood vessels are fragile, incompetent (unlike normal vessels) and can lead to a vitreous hemorrhage or tractional retinal detachment.
A vitreous hemorrhage is a bleed in the back of the eye caused by blood leaking from newly formed vessels. They can be small and cause no symptoms or they can be large and fill the back of the eye causing vision loss.
Symptoms: painless vision loss, a cob-web in your vision, seeing through a red “blob”, new onset floaters, the blood may settle causing better vision after rest and worsening with activity
A tractional retinal detachment can form when new blood vessels grow on the back of the retina. They provide a scaffolding for membrane formation and when these new blood vessels shrink or contract, they can tug on the retina causing a detachment. If the detachment is not in the central part of the vision, you may not notice any symptoms, but if the detachment advances your central vision can be affected.
The other reason a retina surgeon may recommend surgery in a diabetic is for chronic macular edema or swelling of the retina. By removing the vitreous gel in the back of the eye it may result in increased oxygen levels and lead to improvement of macular swelling.
What happens during surgery? What is a vitrectomy?
Our surgeries are performed across the street from our main office at the Valley Surgery Center. They are out-patient procedures, meaning you do not need to be hospitalized, and can go home the same day. After checking in, you will be evaluated by a nurse and an IV line started. The eye undergoing the procedure will be dilated so that the surgeon can view the back of the retina under the operating microscope.
You will meet with our anesthesia team who will discuss your general health and administer medication to keep you calm and relaxed. Once back in the operating room you will be laid on your back for the duration of the procedure. The anesthesiologist will “put you to sleep” for just a few seconds while the surgeon numbs your eye with an injection. This injection will ensure that you have minimal discomfort and that your eye will not move during the operation. The procedure you will have is called a vitrectomy, see below. In basic terms, a vitrectomy is the removal of the gel substance from the back of your eye.
Next, three small cannulas will be inserted into the white part of your eye. One will infuse fluid to keep your eye pressurized, one will allow the surgeon to put a light source in your eye so he can visualize the back of your eye, and the final cannula is used for a device that removes/cuts the gel or blood from your eye.
In cases of vitreous hemorrhage, all of the blood and gel will be cleared from the back of the eye. Your surgeon may apply laser treatment at this time to prevent more bleeding in the future. Your surgeon may or may not leave a small gas bubble in your eye to prevent more bleeding and to help seal the wounds on the white part of your eye.
In the case of a tractional retinal detachment, all of the gel substance will be removed from the back of your eye as well. Next the surgeon will use small forceps to remove any membranes causing the retina to be elevated or detached. The surgery is complete once all of the tugging forces on the retina are relieved and the retina is relaxed. Your eye doctor may add laser to the back of your eye to prevent future detachments and may add a short acting gas to fill the eye cavity. This gas will help keep the retina attached while your eye recovers. In some cases the surgeon needs to fill the back of the eye with oil to keep the retina attached.
Outcomes:
Most patients with relatively good vision before experiencing a vitreous hemorrhage (or bleed) have good visual outcomes. Even in patients with poor vision, before bleeding in the vitreous, can benefit by clearing the blood out surgically and allowing more light to reach the retina.
Patients with tractional retinal detachments are some of the hardest cases for even the best retinal surgeons to perform. Having a tractional retinal detachment means that your eye is already very sick. It can be estimated that with successful surgery that somewhere between ~30-50% of patients may experience improved vision, 20-30% can have stabilized vision (not worsening) and that 20-30% of patients will have worsening of vision. Each patient and surgery is unique, talking to your surgeon during your consultation can give you the best estimates for success based on your circumstance.